Create Rational Quantity Limits For Specialty Drugs
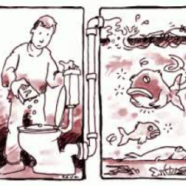
Any Plan that wants to control its prescription coverage costs needs to control the “days supply” of Specialty Drugs that will be dispensed by its PBM. Your Plan can’t afford to squander precious money on Specialty Drugs that your Plan beneficiaries may never use and may instead flush down the toilet. Therefore, if you haven’t […]
Read MorePull Back the Curtain on Manufacturers’ and Switch Operators’ Efforts To Undermine Your Plan’s Cost Savings Efforts
Like most health plans, your plan may be doing all it can to steer your plan beneficiaries to use lower-cost drugs. But manufacturers are paying switch operators (like Relay Health and Change Healthcare) to foil your efforts. If you don’t know what switch operators are or what they do – or your plan is not taking steps to counter switch operators’ machinations – you need to read this article.
Read MoreDon’t Be Fooled By Eli Lilly’s & Express Scripts’ New Diabetes Program
In December 2016, Eli Lilly and Express Scripts announced a new diabetes treatment program to provide 40% discounts on three Lilly diabetes drugs. But the program is anything but what it appears. We explain why in this article, and provide recommendations for health plans and our media friends.
Read MoreDon’t Be Duped By Manufacturers’ Single Digit Price Increase Pledges
Two manufacturers – Allergan and Novo Nordisk – recently won headlines when each vowed to limit the company’s annual drug price increases to single digit numbers. But such increases are anything but laudatory. We explain why in this article.
Read MoreIt’s Time To Stop Paying For Drugs That Were Never Even Approved By The FDA
Approximately 100 years ago, at the turn of the twentieth century, anyone could market any concoction claiming it solved any – or every – health problem. You may think that federal laws now prohibit the distribution of un-approved FDA drugs, but your assumption is dead wrong!
Moreover, you may have told your PBM – or insurer – that your health plan only covers FDA-approved drugs, but you are probably spending a small fortune for drugs that were never submitted to – let alone approved by – the FDA.
Read MoreEnd Unnecessary Costs From Your PBM’s Refill Pill Mill
PBMs’ refill practices are causing health plans to spend hundreds of thousands – or millions – of dollars for pills that will never be used. Every health plan should investigate its PBM’s refill practices, and insist they be changed.
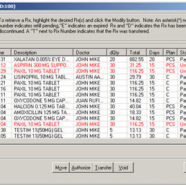
Read MoreBeware of Claims Data Errors – They Have Serious Implications!
It’s critically important that every health plan monitor its claims data to determine whether pharmacy claims data errors are allowing your PBM to overcharge for drugs and misrepresent whether it satisfied your PBM contract’s financial guarantees.
Your PBM has every reason to ignore all claims data errors. And your auditor may do so as well! But your Plan can’t ignore these errors, if you expect to control your costs.
Read this article and understand why.
Read More