If your Plan is like most Plans in the country, you are spending a small fortune on Abilify, even though Abilify lost its patent  protection in 2015 and a generic equivalent is available at far lower cost.
protection in 2015 and a generic equivalent is available at far lower cost.
Your Plan is also likely spending even more on Crestor, which will lose its patent protection in May 2016. And then there’s Zetia, Benicar and Seroquel XR: Each is running up significant costs for Plans, and all will likely lose patent protection before 2016 ends.
Review the reports that your PBM is providing to your Plan that reflect your Plan’s “Top 50” drug costs, and you’ll very likely find Abilify, Crestor and Zetia on the list. If your PBM generates information beyond the “Top 50,” you’ll likely spot Benicar and Seroquel XR among your “Top 200” drug spends.
Better yet, perform your own high-to-low cost “sort” of your claims data, and determine for each of these drugs: (i) its “ranking” in total cost; (ii) your Plan’s total annual costs for each drug; and (iii) your Plan’s average cost per 30 day script for each drug.
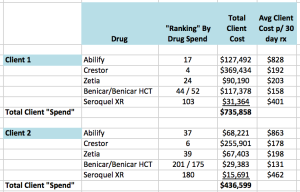
We recently conducted such an analysis for clients that retain our firm to provide ongoing services. Here are the findings for two such clients with total annual drug “spend” (on the PBM side), respectively, of approximately $13.04 million and $12.6 million:
Clearly, these 5 drugs are generating an enormous annual “tab” for both these groups. To be specific, for the two groups, respectively, just these 5 drugs constitute 5.6% and 3.4% of their total annual drug “spend”! Undoubtedly, if you analyze your own Plan’s claims data, you’ll discover similarly shocking figures.
Note too that it’s reasonably likely that if you do nothing whatsoever in connection with these drugs, your Plan’s total costs for each of these brand drugs will dramatically increase in the period immediately before – and after – the brand drugs lose their patent protection. Here’s why:
In other industries, the makers of products typically lower their prices when they are about to face – or already facing – competition; However, in the prescription drug industry, the opposite occurs. For example, knowing that blockbuster Lipitor was about to lose its patent protection in December 2011, its manufacturer, Pfizer, raised Lipitor’s price by 17.5% in 2011.(1) During 2012, as generics entered the market, Pfizer again raised its price by another 9.9%, adding an additional $201 to the average annual cost of therapy.(2)
Pfizer’s actions related to Lipitor were not atypical. In fact, prescription coverage experts who have studied manufacturers’ pricing patterns have concluded that “the retail prices of brand name drugs increase markedly just prior to patent expiration and continue to increase post-patent expiration, albeit at substantial but less rapid rates.”(3)
Bear in mind, too, that manufacturers typically stop paying rebates on brand drugs when competitive generics enter the market, or relatively soon thereafter. Whenever the rebate loss occurs, the total cost of the brand drugs is effectively higher for your Plan.
Tellingly, many brand manufacturers also take certain steps to ensure their higher-cost brand drugs retain their market share even after the brand drugs lose patent protection and generic equivalents become available. Among other strategies, manufacturers frequently increase the dollar value of coupons to reduce – or entirely eliminate – beneficiaries’ “cost share” for the higher-cost brands and thus incentivize beneficiaries to continue to use those drugs.
For all the above reasons, it’s critically important that every Plan – including yours – quickly takes advantage of lower-cost generics when brands lose their patents. As of the writing of this article: Abilify lost its patent protection last year, and numerous generic manufacturers are already selling the generic equivalent – aripiprazole – at up to 75% lower costs than Abilify. Crestor will lose its patent protection in May 2016. And the other 3 drugs will likely face generic competition before the year ends.
If you track the costs of each generic equivalent as it enters the market – and you take action as soon as you know a new generic has lower costs than its equivalent brand – your Plan can save considerable money.
Why You Need to Track the Costs of Newly Available Generic Drugs
To understand why it’s necessary to track the costs of each generic equivalent as it enters the market, you need to understand some basics about the pricing of newly available generic drugs.
When brand drugs lose their patents, typically, only one generic manufacturer produces a generic equivalent of the brand drug during the initial 180 days after the brand drug’s patent loss. As a result, during that “180 day exclusivity period” the price of the only available generic drug typically remains high.
However, as the end of the 180 day exclusivity period approaches, the price of the generic begins to fall, and after the 180 day period ends and several additional generic manufacturers enter the market, the price typically plummets.
Therefore, whenever your Plan determines that a newly available generic is being sold at lower cost than its equivalent brand, that is the time when your Plan should act to limit your Plan’s financial exposure to the generic drug’s cost.(4) You can do so in either of two ways:
First, you can end coverage for the brand drug entirely.
Second, you can implement (what is known as) a Mandatory Generic Program, where you still allow your Plan beneficiaries to use the high-cost brand when the lower-cost generic becomes available, but you require your beneficiaries to cover the differential costs between the brand and the generic equivalent, as well as pay the brand copay.
There are advantages and disadvantages to each of these approaches.
With either approach, your Plan will “cap” its financial exposure at the cost of the generic drugs, unless you allow “medical exceptions” to be made.(5) However, the two approaches differ in their impact on beneficiaries:
If you exclude coverage for the brands, you will eliminate “choice” for your beneficiaries, but there will only be a single moment in time when your beneficiaries experience the disruption of your coverage “block.” Thereafter, your beneficiaries will incur only the generic copay, and your Plan costs will continually decrease as the generic prices fall.
In contrast, if you implement a Mandatory Generic Program, you provide your Plan beneficiaries with “choice,” but those beneficiaries who choose to continue to use the brand drug will experience ongoing disruption: As the price of the generic equivalents fall over time, the beneficiaries will need to pay an increasing amount each time they purchase the drug. As a result, while this latter approach providing “choice” may be more appealing at first glance, it may lead to more complaints and greater dissatisfaction over time.
A Warning About PBMs’ Failure To Adjust Generic Drug Prices Quickly
It’s important to note that you should do more than track the prices of newly available generic drugs in your claims data. You should also track each of the new generic drug’s “Average Acquisition Costs” (AACs) at retail pharmacies. Or, alternatively, you should investigate each of the generic drug’s prices at a low-cost pharmacy like Costco that sells drugs at just above the pharmacy’s acquisition cost.
Why? Because you need to track each of the generic drug’s actual available costs as they fall to ensure your Plan will fully benefit from the drug’s decreasing costs. And many – if not most – PBMs fail to take advantage immediately of plummeting generic drug prices. In fact, after generic drug prices fall dramatically, some PBMs take several months to adjust their generic drug prices on client invoices, while other PBMs fail to do so for a far longer period of time.
In some instances, your PBM’s failure to adjust your invoiced prices may be due to its failure to decrease its reimbursement rates to retail pharmacies, which means the retail pharmacies are making an extra profit “spread” from the PBM’s delayed response. In other instances, your PBM may reduce its reimbursements to retail pharmacies, but continue to invoice your Plan at higher prices, which means the PBM will retain an additional profit “spread” for as long as it fails to act.
But regardless of the delay’s cause – and which entities are profiting from it – your Plan will not fully benefit from the decreasing costs of the generic drugs, if your PBM fails to track those reduced costs when invoicing your Plan.
How can you ascertain whether your PBM is acting effectively? Check your claims data and determine the amounts your PBM is currently invoicing your Plan for the generic equivalent of Abilify – aripiprazole. You may find your prices are still over $400 per 30 day script. That’s far too high given that the drug’s Actual Acquisition Cost (AAC) for retail pharmacies currently ranges from $178 to $350 (depending on the dosage level), and Costco’s price is $173 per 30 day script for each of the two dosage levels it sells.
Knowing of the above problem, our firm included a provision in the National Prescription Coverage Coalition’s PBM contract that makes clear that if our Coalition discovers that the PBM is failing to provide available low pricing for newly available generic drugs, our Coalition is entitled to negotiate better pricing for any such drugs. Our firm also requires a similar contract provision from all PBM contestants when we conduct PBM RFPs for our clients.
But please note that even if your Plan’s PBM contract does not contain such terms, you should still (i) track AAC or Costco prices of each of the generic drugs as they fall; (ii) check your claims data to determine the prices your PBM is invoicing you; and (iii) tell your PBM that you expect to see lower prices, assuming you discover you are being charged too much.
Conclusion
The loss of patent protection on commonly used and expensive brand drugs presents a significant savings opportunity for every Plan.
Take advantage of that opportunity immediately in connection with Abilify. For each of the other 4 drugs mentioned in this article, track the costs of the replacement generics as they enter the market, and either block the brands – or implement a Mandatory Generic Program – as soon as the generic prices are below each of the brand equivalent’s prices. Simultaneously make sure that your PBM is invoicing your Plan at the prices that are available in the marketplace. And then undertake the same efforts, in the coming years, as more such opportunities to save await you in the future.
# # #
To read other Rx Drug Alerts, go here.
Footnotes:
(1) Leigh Purvis and Stephen Schondelmyer, “Rx Price Watch Case Study: Efforts To Reduce The Impact of Generic Competition for Lipitor,” AARP Public Policy Institute. See http://www.aarp.org/content/dam/aarp/research/public_policy_institute/health/2013/lipitor-final-report-AARP-ppi-health.pdf
(2) Ibid.
(3) Leigh Purvis and Stephen Schondelmyer, “Rx Price Watch Report: Retail Prices for Widely Used Brand Name Drugs Increase Considerably Prior to Generic Competition,” AARP Public Policy Institute. See http://assets.aarp.org/rgcenter/ppi/health-care/i49-rx-2011.pdf.
(4) When deciding when to act, each Plan may also want to factor in the difference in copays between brands and generics, which will impact when the Plan will begin to realize savings.
(5) Note that if you block brand coverage – but allow medical “exceptions” to be made – some doctors will undoubtedly request such exceptions, meaning your Plan may pay for the cost of the brands in some instances. The same may be true for a Mandatory Generic Program, if you decide to cover the cost of the brand drug if a doctor submits a valid “medical exception.”