Recent MS Drug Developments Demonstrate Plans Should Obtain Customized Formularies ASAP
Feb 17, 2021How Long Is Your Plan Willing To Throw Away Thousands of Dollars Per Script For An MS Drug? ____________ Review your Plan’s most expensive therapeutic categories, and it’s virtually certain you’ll find multiple sclerosis drugs among those that are ringing up the largest tab for your Plan, even though it’s estimated that less than 1 million […]
Read MoreRequire Your PBM To Take Action on Zytiga
Jan 10, 2019If your Plan wants to decrease and control its costs, you need your PBM to take advantage of every Specialty Drug savings opportunity. Unfortunately, many – if not most – PBMs fail to do so. Zytiga, a high-cost treatment for metastasized prostate cancer, now has a far lower-cost generic substitute available, called abiraterone. Litigation hangs […]
Read MoreCreate Rational Quantity Limits For Specialty Drugs
Jul 24, 2018Any Plan that wants to control its prescription coverage costs needs to control the “days supply” of Specialty Drugs that will be dispensed by its PBM. Your Plan can’t afford to squander precious money on Specialty Drugs that your Plan beneficiaries may never use and may instead flush down the toilet. Therefore, if you haven’t […]
Read MoreDecreasing Drug Costs – Here’s How We Achieved Them
Apr 08, 2018We’re thrilled to report yet again that the National Prescription Coverage Coalition has achieved striking savings for our Coalition Members.
Based on year-end analyses, our Coalition Members decreased their prescription coverage costs by approximately 20% to 30%.
Read MoreMore Drug Price Increases
Mar 19, 2018Remember when several drug manufacturers promised last year to limit their drug price increases to single digits and claimed other drug manufacturers drastically increasing their drug prices were “outliers”? If those manufacturers’ words made you think the days of price gouging were over, think again.
Read MoreYour Plan Can Decrease Its Prescription Coverage Costs (But You Need To Take Action To Do So)
Jan 15, 2018We’re thrilled to report yet again that the National Prescription Coverage Coalition has achieved striking savings for our Coalition Members. Based on year-end analyses, our Coalition Members decreased their prescription coverage costs by approximately 20% to 30%. Sound too good to be true? It’s not. These savings resulted from our Coalition Members implementing dozens of ongoing recommendations provided by our Coalition experts, such as: […]
Read MoreAct Now – Block Lyrica CR Preemptively
Nov 17, 2017If your Plan wants to control its prescription coverage costs – and minimize disruption to your plan beneficiaries – your Plan needs to act preemptively to block certain drugs before they even enter the market. Lyrica CR exemplifies why.
Read this to understand Pfizer’s – and other manufacturers’ – ploys that prevent your Plan from saving money from generic drugs. And learn how you can counter manufacturers’ strategies by blocking certain newly-approved, but entirely unnecessary, drugs before your Plan beneficiaries start taking them.
Read MorePlan Administrators: Limit Your Restasis Coverage
Oct 05, 2017If you missed the latest example of drug manufacturer abuse, you need to learn about Allergan’s Restasis antics, understand your Plan’s resulting costs, and take action in response.
Why? Because you’ll not only save your Plan considerable money by acting on a single drug, you’ll also help teach Allergan a much-needed lesson and discourage other manufacturers from engaging in similar abuses.
Read MorePlan Administrators and Fiduciaries: It’s Time To Take REBATE ACTION – File An Accounting Procedure!
Jul 10, 2017As newspaper articles multiply describing PBMs’ questionable rebate conduct, every Plan administrator and fiduciary should consider filing a lawsuit against your PBM seeking an “accounting”. As a Plan administrator or fiduciary, you’re charged with ensuring your Plan receives all monies your Plan is entitled to receive. Moreover, through an accounting, you’re likely to discover your PBM has been hiding large amounts of monies that, if reimbursed, would significantly decrease your Plan’s costs. And given the amounts your Plan may recover, you’ll likely be able to locate a law firm to file a lawsuit on a contingency basis, meaning the litigation won’t cost your Plan a dime.
Read MoreExpress Scripts’ Lawsuit Reveals Striking Information About PBM Rebates
May 31, 2017For years, PBMs have consistently refused to disclose any information about their secret “deals” with manufacturers to obtain “rebates” – that PBMs presumably pass through – and “other monies” – that PBMs collect from manufacturers but PBMs may retain for themselves.
But now, a new lawsuit filed by Express Scripts against the drug manufacturer kaleo reveals at least some information about Express Scripts secret deals. And the information is shocking. Express Scripts is clearly collecting mega-millions of dollars from manufacturers, and much of that money is labeled “administrative fees” and “price protection rebates” that Express Scripts may not be entirely passing through to its clients or the federal government. Every Plan administrator and fiduciary – and the federal government – should insist on learning more about the millions that Express Scripts and other PBMs are collecting.
Read MoreWant To Decrease Your Rx Coverage Costs? Pay Attention to Horizon Pharma’s 1st Quarter Report
May 15, 2017Horizon Pharma – the manufacturer of three extremely expensive drugs – Vimovo, Duexis and Pennsaid – just released its Quarterly Earnings Report causing its stock to plummet. The Report should cause every Plan to stop providing coverage for all 3 of these drugs and stop relying on its PBM’s “standard” Formulary.
Read MoreStriking Savings Are Possible (But Your Plan Needs To Act To Obtain Them)
Apr 30, 2017We’re thrilled to report that yet another Coalition Member that followed our Coalition’s recommendations and took aggressive steps to control its prescription coverage costs has now achieved a 16% cost decrease.
Read MorePull Back the Curtain on Manufacturers’ and Switch Operators’ Efforts To Undermine Your Plan’s Cost Savings Efforts
Jan 11, 2017Like most health plans, your plan may be doing all it can to steer your plan beneficiaries to use lower-cost drugs. But manufacturers are paying switch operators (like Relay Health and Change Healthcare) to foil your efforts. If you don’t know what switch operators are or what they do – or your plan is not taking steps to counter switch operators’ machinations – you need to read this article.
Read MoreDon’t Be Fooled By Eli Lilly’s & Express Scripts’ New Diabetes Program
Dec 21, 2016In December 2016, Eli Lilly and Express Scripts announced a new diabetes treatment program to provide 40% discounts on three Lilly diabetes drugs. But the program is anything but what it appears. We explain why in this article, and provide recommendations for health plans and our media friends.
Read MoreDon’t Be Duped By Manufacturers’ Single Digit Price Increase Pledges
Dec 21, 2016Two manufacturers – Allergan and Novo Nordisk – recently won headlines when each vowed to limit the company’s annual drug price increases to single digit numbers. But such increases are anything but laudatory. We explain why in this article.
Read MoreMessage from Mylan: Pay Attention to Rebates
Nov 17, 2016In recent testimony before a House Committee, Mylan’s CEO asserted that $334 of EpiPen’s list price of $608 – or 55% of the total $608 – could be attributed to PBMs and three other drug channel vendors extracting payments from Mylan.
Soon, other evidence emerged reflecting manufacturers’ price increases related to diabetes and rheumatoid arthritis drugs might be related to PBMs’ rebate activities. These new developments make clear that every Plan administrator needs to understand the complex world of drug manufacturer rebates and other payments, and develop strategies that will address these issues.
Read MoreTake Action To Decrease Your Plan’s Crestor Costs
Nov 17, 2016If you examine your Heath Plan’s claims data, it’s extremely likely you’ll discover that Crestor is costing your Plan a small fortune. Typically, Crestor represents more than 1% of a Plan’s total annual drug costs. As a result, Crestor almost always appears on a Plan’s list of “Top Twenty Most Expensive Drugs.” Frequently, Crestor is among the “Top Ten” – jockeying to collect even more money from Plans than many high-cost specialty drugs.
But as if manna has fallen from heaven, there is now a means to reduce your Health Plan’s costs. Details can be found in this article.
Read MorePay Attention to Your Metformin HCL ER Diabetes Costs
Oct 30, 2016We regularly review our clients’ claims data to detect issues that, if corrected, can reduce our clients’ costs without harming their plan beneficiaries’ drug access. Read this short article about metformin HCL ER, and you’ll understand what we’re doing, and what every health plan can – and should – do as well.
Read MoreAdditional Information About New Drugs’ Dangers
Oct 09, 2016We received multiple requests for additional information after we published our last article describing new drugs’ dangers based on recent developments related to hepatitis C drugs. Accordingly, we have written another brief article providing additional information reflecting why all health plan administrators should exclude – or limit – coverage of many new drugs.
Read MoreProtect Your Plan Beneficiaries From New Drugs’ Dangers
Oct 06, 2016The latest FDA Black Box Warning about hepatitis C treatments demonstrates why it’s imperative that your Plan implement methods for protecting your beneficiaries against the dangers of new drugs.
After all, more than three years after the FDA approved the first of eight new hep C treatments, the FDA has just issued yet another warning about a newly discovered danger related to these drugs.
Read MoreDoes Your Health Plan Actually Need the Large Chain Pharmacies In Your Retail Pharmacy Network? (The Short Answer is “No!”)
Sep 25, 2016Most health plans’ prescription coverage programs allow plan beneficiaries to purchase drugs at virtually all retail pharmacies in the United States, regardless of the prices charged by those pharmacies.
But in a time of spiraling drug costs, every health plan administrator should consider excluding either – or both – of two of the highest-cost chain pharmacies: CVS and Walgreens. Read this article to find out why.
Read MoreAre You Taking Action To Protect Your Health Plan Against Extreme Drug Price Increases?
Jun 22, 2016You’ve undoubtedly heard that Turing Pharmaceuticals purchased a low-cost drug, Daraprim, and raised its cost by 5433% last year. And Turing’s smug CEO, Martin Shkreli, defended the price hike as perfectly reasonable. But are you aware that several other drug manufacturers are continually purchasing drugs and dramatically increasing their prices? And do you know that during the past 12 months the prices of almost 150 brand drugs increased by 100% or more?
Most important of all: Do you realize that as your Plan’s administrator, you can take steps to protect your Plan against some of these outrageous price increases? Read this article to learn how to do so.
Read MoreIt’s Time To Stop Paying For Drugs That Were Never Even Approved By The FDA
May 26, 2016Approximately 100 years ago, at the turn of the twentieth century, anyone could market any concoction claiming it solved any – or every – health problem. You may think that federal laws now prohibit the distribution of un-approved FDA drugs, but your assumption is dead wrong!
Moreover, you may have told your PBM – or insurer – that your health plan only covers FDA-approved drugs, but you are probably spending a small fortune for drugs that were never submitted to – let alone approved by – the FDA.
Read MoreJust How Much Is Your Plan Spending On Abilify – and Other Drugs – That Have Recently Lost – Or Will Soon Lose – Their Patent Protection ?
Apr 27, 2016If your Plan is like most Plans in the country, you are spending a small fortune on Abilify, even though Abilify lost its patent protection in 2015 and a generic equivalent is available at far lower cost. Your Plan is also likely spending even more on Crestor, which will lose its patent protection in May 2016. And then there’s Zetia, Benicar and Seroquel XR: Each is running up significant costs for Plans, and all will likely lose patent protection before 2016 ends.
It’s time for your plan to stop squandering money on high-cost brand drugs that have lost their patents! We explain exactly what you can do to control your costs here.
Read MoreEliminate – Or At Least Decrease – Your Rx Coverage Costs For Proton Pump Inhibitors
Mar 17, 2016Virtually all health plans are spending a large sum of money covering Proton Pump Inhibitors – drugs like Nexium, Prilosec and Prevacid, and their generic equivalents (esomeprazole, omeprazole and lansoprazole). Simply stated, health plans are wasting their money doing so.
Read this detailed article that will help you understand exactly how to eliminate – or at least significantly reduce – your Proton Pump Inhibitor costs.
Read MoreIs Your Health Plan Controlling Its Testosterone Use?
Feb 24, 2016Spend a few minutes studying your health plan’s claims data, and you’ll very likely discover your plan is spending large sums of money on men’s testosterone products.
In fact, you’ll likely discover your plan is spending several thousand dollars a year for each male beneficiary who is choosing to rub gel into his shoulders in the hope that the gel will enhance his sexuality.
But numerous previous studies – and an article in last week’s New England Journal of Medicine – make clear that covering testosterone products not only squanders your plan’s limited assets, but also subsidizes dangerous medical practices of dubious medical utility.
For an in-depth examination of the testosterone problem – and why you should take steps to address it – read this article. We’ll also provide a detailed description of precisely the steps you should take.
Read MoreAre You Protecting Your Health Plan Against Astronomical Drug Price Increases?
Sep 27, 2015Drug prices were in the news this week because of a shocking 5000% increase in the cost of a single drug: Daraprim. But during the first 9 months of 2015, the average wholesale price (AWP) of almost 50 drugs more than tripled.
Given this striking fact, unless your plan – or Coalition – positions itself to learn about – and respond to – these steep price increases, as well as those that will inevitably occur in the future, your plan will not be able to control its costs. Read this article, to find out exactly how to do so.
Read MoreThe Frightening Implications of Farydak & Kalydeco
Jun 13, 2015During the first six months of 2015, the FDA approved more than a dozen new high-cost Specialty Drugs. Two of those drugs – Farydak & Kalydeco – reflect the frightening financial implications of new specialty drugs, and steps every health plan should take to control their costs.
Read MoreHere’s How To Investigate – And Then Cure – Your Hep C Drug Cost Problem
Apr 24, 2015HR Execs: You’ve undoubtedly read about PBMs’ purported hep C manufacturer “shake-down,” which PBMs claim decreased health plans’ costs for hep C drugs.
But it’s reasonably likely that your plan didn’t actually receive any benefit from PBMs’ purported shake-down. In fact, it’s reasonably clear that only the PBMs actually benefited from their secret manufacturer deals.
To understand why your hep C costs are probably as high – or even higher – than they were before PBMs’ actions, read this article. We also describe what you should do to control your hep C costs.
Read MoreEnd Unnecessary Costs From Your PBM’s Refill Pill Mill
Mar 21, 2015PBMs’ refill practices are causing health plans to spend hundreds of thousands – or millions – of dollars for pills that will never be used. Every health plan should investigate its PBM’s refill practices, and insist they be changed.
Read MoreHR Execs: Take Note Of Hepatitis C Realities
Jan 08, 2015For health plan execs that want to control their prescription coverage costs, recent hepatitis C developments provide critical lessons.
Read MoreMake Sure Your Plan Continuously Monitors – and Responds to – Newly Approved Rx Drugs !
Oct 21, 2014The “Latest” Is Not Necessarily The “Greatest” When It Comes To Drugs
The drug marketplace is continually changing, and new drugs are continually entering the market.
But there’s good reason to act to prevent your plan beneficiaries from using many newly approved drugs.
Read this article and learn why doing so will often protect – not harm – your Plan Beneficiaries, as well as conserve your Plan assets. And why you can’t depend on the FDA – or your PBM – to accomplish those goals.
Read More
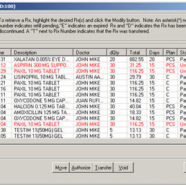
Beware of Claims Data Errors – They Have Serious Implications!
Aug 13, 2014It’s critically important that every health plan monitor its claims data to determine whether pharmacy claims data errors are allowing your PBM to overcharge for drugs and misrepresent whether it satisfied your PBM contract’s financial guarantees.
Your PBM has every reason to ignore all claims data errors. And your auditor may do so as well! But your Plan can’t ignore these errors, if you expect to control your costs.
Read this article and understand why.
Read MoreControlling Compound Drug Costs
Apr 15, 2014Rx Alert – May 2014
Careful monitoring of new clients’ claims data reveals an abundance of new, high cost Compound Drug creams that are causing Plans’ costs to soar. And many – if not most – of the new compound drugs have no proven efficacy!
Read this article to understand the problem, and learn exactly what you need to do to ensure these compound drugs don’t cost your Plan immense sums.
Read More