Virtually all health plans are spending a small fortune covering Proton Pump Inhibitors – drugs like Nexium, Prilosec and Prevacid, and their generic equivalents (esomeprazole, omeprazole and lansoprazole).
Virtually all health plans are spending a small fortune covering Proton Pump Inhibitors – drugs like Nexium, Prilosec and Prevacid, and their generic equivalents (esomeprazole, omeprazole and lansoprazole).
Unfortunately, almost no PBMs are bothering to tell their clients how they can eliminate – or at least decrease – their Proton Pump Inhibitor costs. Therefore, health plans need to educate themselves and take steps on their own to protect their assets, as well as their members’ health.
Here’s how to do so.
Cost Overview
Proton pump inhibitors, also known as PPIs, are drugs that are used to treat heartburn, gastroesophageal reflux disease (GERD) and gastric ulcers.
In 2001, the leading PPI – the famous “purple pill” known as Prilosec – lost its patent. Immediately thereafter, its generic equivalent (omeprazole) became available at a far lower price, both as a generic and an over-the-counter drug (OTC). Unfortunately, through a massive marketing campaign, Prilosec’s manufacturer moved many Prilosec users to a slightly different version of the drug – called Nexium – the “new purple pill” – shifting the market away from generic or OTC omeprazole to the new, high-cost brand drug Nexium. (1) As a result, Nexium became the next PPI racking up billions of dollars of annual drug sales.
However, in May 2014, Nexium finally lost its patent. Within months, Pfizer added Nexium to several other PPIs that were already being sold as over-the-counter drugs. But despite the availability of numerous low-cost OTC PPIs, manufacturers continue to market their high-cost brand drugs and rack up large revenues. And PBMs help them do so by including the manufacturers’ high-cost drugs on PBMs’ Formularies.
For example, according to Express Scripts Annual Drug Trend Report for 2014, PPIs were the sixth most expensive therapeutic category in 2014, with 23% of scripts still brand drugs, and an average script cost of $56.26. (2) According to Express Scripts’ Drug Trend Report for 2015, PPIs were still the sixth most expensive therapeutic category in 2015, with lower brand drug use (only 7.7%) and lower average script cost ($43.14), but a 35.6% increased per member per year spend. Why? As Express Scripts explained it, a 36.3% increased unit cost had occurred that was “heavily influenced by the branded products like Nexium, Dexilant and Prevacid.” (3)
Tellingly, many, if not most, PBMs – including Express Scripts – continue to include high-cost brand drug PPIs on their Formularies. In Express Scripts 2016 Formulary, Express Scripts included all three of the brand drugs that had driven higher unit costs the previous year: Nexium, Dexilant and Prevacid. In Caremark’s 2016 Formulary, Caremark included Nexium and Dexilant as “preferred products,” even though Caremark excluded 126 other products from its Formulary.
Why do PBMs engage in such questionable practices? The short answer: PBMs are interested in luring in new clients, while simultaneously increasing their profits.
The more detailed explanation: PBMs continue to feature brand PPIs in order to increase the rebates they can provide to their clients, especially given their clients’ ongoing failure to understand that a rebate-able brand drug is almost never as inexpensive as its generic substitute. Meanwhile, PBMs continue to dispense generic PPIs, because PBMs’ profit “spreads” on those generics is often very high, especially given PBMs’ excessive charges for generic drugs. (4)
Making matters worse, given PBMs’ obvious conflicts of interest, many, if not most, PBMs fail to provide their clients with an obvious recommendation: It makes no sense for plans to cover brand PPIs, or even generic PPIs given PBMs’ excessive charges for generic drugs. Plans should stop covering all prescription PPIs, and ask their beneficiaries to rely instead on over-the-counter PPIs. Or plans should only cover certain generic prescriptions – and OTC PPIs – and limit the amount the plans will pay to reasonable dollar amounts. (5)
Comparing Rx & OTC PPI Costs
Early last summer, our firm and our National Prescription Coverage Coalition analyzed the costs of several therapeutic categories for our clients and our Coalition Members. Our goal was to present a series of cost-saving recommendations to all concerned, including for PPIs. Here’s an example of the information we provided to one Coalition Member concerning PPIs:
Analyzing the plan’s previous claims data, we projected it would spend approximately $382,000 for prescription PPIs on an annualized basis. Given that the plan’s total annual costs would likely be approximately $12 million, its PPI costs were not inconsequential.
Clearly, if the plan stopped providing coverage for all prescription PPIs – and asked its beneficiaries to purchase OTC PPIs on their own – the plan would save $382,000. Even if the plan provided coverage of, say, $15 per OTC purchase, the plan would still save approximately $356,000.
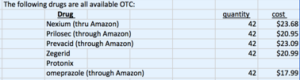
We also pointed out that the plan wasn’t providing coverage for any other OTCs (like aspirin, cough syrup, and numerous other products). And plan beneficiaries could easily access OTC PPIs – including through Amazon – at very low cost, as shown in a Table that we provided:
We also urged the plan to end coverage for two “combo PPIs” that were particularly exorbitant in price: Vimovo and Duexis. Vimovo – a combination of Nexium (esomeprazole) and naproxen (a common NSAID, available as Aleve OTC) – cost about $1,400 per 30 day prescription at the time, and now runs about $1,650 per 30 day prescription. Duexis – a combination of ibuprofen (basic OTC aspirin) and famotidine (OTC Pepcid) – cost about $1,425 per 30 day prescription then, and about $1,650 as of the date of our analysis.
“Why should any plan provide coverage for either drug,” we asked, “when both drugs are nothing but ‘convenience’ drugs that combine two inexpensive OTCs, and charge outrageous prices for doing so?”
Moreover, we recommended against covering the drugs, and limiting any “medical exceptions” through a strict, customized Prior Authorization protocol that we drafted, since it was hard to contemplate any “medical exception” justifying the drugs’ use, especially at such exorbitant prices. After all, plan beneficiaries could obtain the benefits of both drugs simply by taking the two OTC components of each drug separately.
Educate Beneficiaries When You Change Your Coverage
Whenever your Plan decides to change its coverage, an opportunity arises to influence your beneficiaries by providing them with critical information. Our consulting firm and Coalition believe two core messages should be communicated if you eliminate – or reduce – PPI coverage.
First, plans need to explain that everyone must contribute to lowering aggregate drug costs, because drugs are never “free” (despite a widespread belief to the contrary). Beneficiaries need to understand that to the extent a corporation’s or union’s or municipality’s drug coverage costs increase, premiums and copays and deductibles will likely increase too. Moreover, less money will be available for other matters, like salaries, fringe benefits and other programs. Accordingly, for a plan beneficiary to spend $200+ for a 30 day prescription of Nexium – let alone $1,650 for a 30 day script of Vimovo – simply doesn’t make sense when the beneficiary can spend $20 for an OTC substitute.
Second, plan beneficiaries should be provided certain basic warnings about possible PPI overuse. Here’s a short summary of such issues provided by Consumer Reports on Health:
“If you suffer from occasional heartburn and have not been diagnosed with GERD, nonprescription antacids such as Maalox, Mylanta, Rolaids, and Tums, or acid-reducing drugs known as H2 blockers, such as cimetidine (Tagamet), famotidine (Pepcid), nizatidine (Axid) and ranitidine (Zantac) will very likely provide relief. All of those products are available without a prescription….”
“If, however, you experience heartburn twice a week or more for weeks or months on end, have frequent regurgitation of food into your throat or mouth (with or without heartburn), or if your heartburn is not relieved by the drugs mentioned above, you may have GERD and may need a PPI.” (6)
Moreover, everyone who is continually using PPIs should talk with their doctor. Those suffering from heartburn should discuss dietary and lifestyle changes, such as eating smaller meals, losing weight if needed, not lying down for at least 3 hours after eating, and avoiding alcohol. Those taking PPIs should also understand that “several studies have linked PPIs to a higher risk of pneumonia and infection… and other studies have found that long-term use of PPIs may be associated with an increased risk of fractures.” Also, those taking Plavix or clopidogrel to thin their blood after a blood clot or heart attack “should be especially cautious with PPIs … because they can reduce” those blood thinners’ effectiveness, which could increase the risk of another heart attack. (7)
# # #
To read other Rx Drug Alerts, go here.